Read Full Transcript EXPAND
CHRISTIANE AMANPOUR: Hello, everyone, and welcome to “Amanpour and Company” from London. Here’s what’s coming up.
(BEGIN VIDEO CLIP)
DR. TEDROS ADHANOM GHEBREYESUS, DIRECTOR-GENERAL, WORLD HEALTH ORGANIZATION: The window of opportunity is narrowing and the time to act
was actually more than a month ago or two months ago.
(END VIDEO CLIP)
AMANPOUR: I speak to the W.H.O. senior adviser about what can still be done as world leaders finally come together in a virtual Summit.
Then —
(BEGIN VIDEO CLIP)
MARIE-ROSELINE DARNYCKA BELIZAIRE, MEDICAL DOCTOR: I was ready to fight Ebola, but I wasn’t ready to fight against the trauma of this community.
(END VIDEO CLIP)
AMANPOUR: A lesson from the front lines fighting Ebola. After battling the virus in a war zone, the devastated Eastern Congo now braces for a new
threat from coronavirus.
Then —
(BEGIN VIDEO CLIP)
DAVID KESSLER, AUTHOR, “FINDING MEANING: THE SIXTH STAGE OF GRIEF: Our normal life, our routines, seeing people, our work, everything has changed.
(END VIDEO CLIP)
AMANPOUR: Behind the spiking death toll, are individual lives lost. Our Michel Martin speaks with grief.com founder, David Kessler.
And finally, a spiritual balm, an “Ode to Joy.” Playing Beethoven’s ninth and proving that creativity won’t be stifled by social isolation.
Welcome to the program, everyone. I’m Christiane Amanpour in London.
Coronavirus is a global war in urgent need of a global response. And so, an extraordinary virtual global summit took place today, as Chinese president,
Xi Jinping, the U.S. president, Donald Trump, and other G20 leaders finally met via teleconference to unite their efforts towards fighting this
pandemic.
The W.H.O. has been calling for world leadership to share resources and information. Just yesterday, a meeting of the G7’s most powerful economies
fizzled after the United States insisted on playing name and blame games, calling COVID-19 the Wuhan virus.
Meanwhile, the world economy is tumbling towards recession. In the United States, 3.3 million workers filed for unemployment benefits. It’s the
highest number ever reported. But it simply isn’t accurate to say that no one could have foreseen this pandemic as President Trump and some other
leaders claim.
In the United States, war gaming for these catastrophes is a matter of national security and civil defense. And the government had detailed plans
in place. But for some reason, they appeared to be still on the shelf, while precious time has been lost. Now, more than 22,000 people are dead
and almost half a million infected with the disease around the world.
The director-general of the World Health Organization scolded world leaders for not acting fast enough against the pandemic. Now, his chief advisor,
Dr. Senait Fisseha, joins me via Skype from Omaha, Nebraska.
Dr. Fisseha, welcome to the program.
I want to ask you as, you know, you’re involved in this fight against this pandemic, where do you think the world is right now, given, as we’ve said,
the director-general has said that precious time has been lost?
DR. SENAIT FISSEHA, CHIEF ADVISOR TO THE DIRECTOR-GENERAL, WORLD HEALTH ORGANIZATION: Thank you, Christiane, for having me. Certainly, we all are
watching this pandemic escalate and unfold in front of us. The World Health Organization has been warning all of us that this is coming.
Of course, sometimes, when we see epidemics and outbreaks far away from us, it makes it hard to internalize that it can hit us as well. But as Dr.
Tedros always say, you know, pathogens don’t respect borders. And certainly, what we have seen now is massive escalation of the outbreak.
Countries are responding, we’re seeing various kinds of response. Some have taken very aggressive measures of social distancing and lockdown and others
have combined that with aggressive testing and were making progress.
But as he alluded to just yesterday, the window is narrowing and we need to see more solidarity, more coordinated global response and leadership and
more aggressive measures taken, particularly around public health measures of finding the cases, testing them, isolating them, treating them and doing
contact tracing.
AMANPOUR: Dr. Fisseha, do you think, from what you know, that this call for leadership has now sort of taken place via teleconference? Do you think
the G20 meeting will signify a significant uptick in coordinated response to this?
FISSEHA: So, you know, Christiane, the World Health Organization is the only entity in the world that is mandated for the health and well-being of
7 billion people in about 194 member states plus some territories. And under Dr. Tedros’ leadership, they have done a fantastic job trying to do
that. But it also falls in countries in stepping up and showing leadership.
And, you know, Dr. Tedros, since he took the helm of the W.H.O., has been calling that, you know, pandemics are going to happen. And the G20 has been
going through all the pandemic exercises. We are just still on the heels of Ebola and DRC and recovering from the West Africa Ebola outbreak that took
the lives of about 11,000 people between 2014 and 2016. But somehow, he’s not sounding, you know, the alarm loud enough. I mean, there have been
exercises, but not the kind of global solidarity we want to see.
Part of this is that, now is not the time to, you know, play blame game or point fingers, as he clearly articulated yesterday and has said many, many
times, public enemy number one is the virus. So, how do we get countries to get together, show global solidarity, use the W.H.O. to coordinate, share
data, get necessary life-saving interventions to the people and especially front-line health care providers who need it the most, get testing to
countries, especially those countries that are very — have a very weak health system and are in conflict or have large internally displaced
people? This is what we need to do.
And Dr. Tedros has been doing that, ensuring that, you know, our world leaders are committing. He’s reaching out to everyone. He’s engaging world
leaders. He absolutely believes this is a matter of political will and political commitment. So, he is reaching out to every leader, health
ministers, foreign ministers, to take a whole of government approach in a very cohesive and strategic way.
AMANPOUR: So, as you said, this is public enemy number one, said Dr. Tedros. We’re going to play a little bit of what he did say yesterday about
the narrowing window of opportunity, but that there may be some kind of potential second chance. Let’s just play this and we’ll ask you to talk
about it.
(BEGIN VIDEO CLIP)
DR. TEDROS ADHANOM GHEBREYESUS, DIRECTOR-GENERAL, WORLD HEALTH ORGANIZATION: This virus is public enemy number one. It’s a dangerous
virus. And we have been saying to the world that the window of opportunity is narrowing. And the time to act was actually more than a month ago or two
months ago. That’s what we have been saying. But we still believe that there is opportunity. I think we squandered the first window of
opportunity, but we’re saying today, my message, I made it clear that this is a second opportunity, which we should not squander.
(END VIDEO CLIP)
AMANPOUR: So, Dr. Fisseha, what is he saying about squandering? Which country squandered? Did every country squander? And how does he reckon that
there is a second window of opportunity, precisely?
FISSEHA: So, I think if we take a step back and, you know, take sort of a higher altitude picture of what has been happening since December, W.H.O.
has been able to gather enormous amount of data, how this disease is working, how’s the outbreak, how fast is it replicating, what’s the
transmissibility and what are some of the measures that are affected.
So, although, as he clearly articulated that W.H.O. has been, you know, sounding the alarm, not everyone has taken the same radical, aggressive
measures some other countries have taken. So, what he’s really saying is, let’s really focus on the virus. Let’s look at the scientific evidence
available to us. Let science guide us, and based on the information we have, figure out a strategy that is a mix of, you know, distancing, social
distancing, lockdown. That is only half of the puzzle.
As I said earlier, that needs to be coupled with — you know, what he was really articulating yesterday is social distancing is critical to reduce
the virus’ transmissibility, but it’s not going to get rid of the virus. So, what we need to do is take really aggressive measures moving forward.
And he is, again, like I said, the mutual has been at the forefront of gatherings information, sharing information, convening experts and getting
supplies and products to countries, especially those countries who need it the most.
So, I think what he’s saying is, yes, we’ve lost a lot of lives. And, you know, for Dr. Tedros, a loss of life is not just numbers. I mean, here is a
guy a health minister of Ethiopia and has delivered health care for 100 million people in very resource constraint setting. So, he absolutely
understands the struggle, the most vulnerable people are going through and the fragile countries are going through.
So, what he’s saying is, let’s really act, let’s look at the evidence, let’s look at what we’ve learned, let’s build solidarity, let’s get global
leadership, let’s coordinate, because this is not only a public health impact, but for the poorer countries, there’s going to be a massive
economics impact and how can we contain that.
AMANPOUR: We’ll talk about the poorer countries in a moment, but I first want to ask you, because you are in the United States, and there is a fear
that the U.S. will become the next epicenter. Now, as Dr. Tedros has said, there are second opportunities. Don’t squander, you know, what may still be
available to stop this. Is it inevitable that the United States becomes the next epicenter or is there time now to reverse that? And if so, how?
FISSEHA: I don’t think any one of us can tell that. I mean, of course, the rate of infection in the United States has been alarming, but ask Dr. Tony
Fauci, who’s really been leading the scientific community in this fight clearly articulated, it’s going to be the virus that dictates that.
However, our response to contained and mitigate the virus will also have a significant impact. And we are worried, we’re watching the U.S., I mean, as
that front-line health care provider, watching my colleagues struggle with the basics has been enormous.
So, the combination of the lockdown strategies that have been put in place and now, you know, testing kits are becoming a lot more accessible than
they were two weeks ago. We are also seeing firsthand what it means to have our hospitals overflow. What it means to make tough decisions about, you
know, who goes and stays on the ventilators. What it means to take care of patients who have no safety net. So, it has really been a humbling
experience for most of us who have never seen United States in this lens.
But I do fundamentally believe in the resilience of the American people. I think this country has innovated and has come up with incredible — I mean,
the model for public health globally has been adopted from the Center for Disease Control and Prevention. And we have the global experts, we have the
national experts, we have incredible leadership. And I do feel very comfortable — not comfortable, but very hopeful that we will contain this
virus. So, I don’t have another alternative.
AMANPOUR: Right. And W.H.O. has said that if the United States takes aggressive measures, it does have some hope of reversing the trend. So,
what I want to ask you is this. Is there a collision of politics versus medical science? You’ve seen Dr. Anthony Fauci, who said, and you repeated
it yourself just a moment ago, that it’s the virus that makes the timeline, not us. You know, the virus makes the timeline. But President Trump has
said that, you know, he wants the country raring to go by Easter.
Medically, what will that do? And what will be the effect of that if there’s suddenly some kind of opening up of the country?
FISSEHA: So, you know, as a practicing physician, I tend to be guided by evidence and all of my colleagues do the same, and we’re going to do what
the evidence tells us to do. There are countries who have controlled this virus without a massive aggressive lockdown and there are others who have
done a combination of things.
The issue in the United States is going to be once the transmissibility has reached a certain level, you know, you’re going to need a combination of
strategies to move this forward. And the guidance of Dr. Fauci and the community — the scientific community has thus far been spot-on.
What we are worried about in this country right now is access to basic protective equipments like masks and testing kits and access to ventilators
and everyone, private, public, you know, government is doing what they can to keep our front-line health workers safe, to ensure that patients are
getting the care they deserve and they need.
So, I think if we continue on this strategy and learn from other countries as data becomes available and support the industry so that we have more
products in the market for more therapeutics, more diagnostic tools. And frankly, each day we’re learning new things about this virus and we
continue to be guided by that evidence, I do think we will manage.
But we actually are going to need very, very aggressive measures. You know, talking to my friends who are front-line in New York, who are not eating,
who are not taking breaks. I mean, you know, they are posting very, very terrible stories of how their system is completely overwhelmed. They don’t
have access to basic things. They are exhausted mentally, physically, and we need to address that.
AMANPOUR: So, that’s them and then, of course, you’ve got the lack of ventilators and all the other things that you’ve talked about that are now
being ramped up, but there’s a long way to go.
So, look, I want to ask you, because this is clearly a health emergency, which is an economic — you know, the economy has taken a massive hit and
it’s also kind of a national security emergency, as well. And about a hundred national security officials have signed a letter asking the
president to actually enact the War Production Act that he invoked and force or make requisition private companies to join this fight and to turn
their, you know, ability for production towards this fight.
Do you think that should happen? I mean, surely, there’s no time to lose. And that’s built into the response in any crisis in the United States.
FISSEHA: Yes, Christiane, every country is going to do what is important and what is critical to get them where they need to. And the United States
has to do the same. You know, right now, what we know is every day the situation is improving, but we are going to need much more drastic
measures, as you mentioned, to make ventilators and personal protective gears. And the government and the — both at the state level and the
federal level do know what they need to get us there and we want them to act immediately so that health care workers who are really at the highest
risk need the tools — get the tools they need to be able to provide the services that the communities are asking of them.
AMANPOUR: Now, just to pivot a little bit, but not really, I mean, you are a professor of OB/GYN at the University of Michigan. And you are very
concerned about the disproportionate impact on women around the world, of many health crises, but this one especially.
Roughly 70 percent of the global health care workforce is made up of women, according to analysis of more than a hundred countries by the W.H.O. What
are you seeing here in terms of how they’re being affected in this fight?
FISSEHA: Absolutely. You know, as an adjunct faculty at the University of Michigan, I stay in close contact and see what is happening both in the
United States and globally. As you clearly stated, 70 percent of the front- line workforce is women.
Right now, many countries are not reporting data on gender and sex. Of course, we’re getting general information around who’s getting sick and
who’s dying, and that data seemed to suggest there is a higher mortality for men, but that does not tell the whole story.
So, if you look at women as a subset, there are two things that put them at the highest risk. One, as we talked about, is that they’re the front-line
health care providers, particularly when you look at community health workers, nurses. You know, just a few days ago, there was a publication
circulating, there are now countries that are — low-income countries that are trying to do their best to tackle this epidemic — this pandemic, and
they’re having community health workers go house to house trying to identify patients without any protective gears. So, absolutely, that puts
them at a much higher risk.
If you look at the data from China in Hubei, 90 percent of the front-line were women. But the second piece to this is that the data globally shows
that women are also the utilizers — the bigger utilizers of health services, not just for them, but also for their families, elderly,
children. So, they are coming in contact with a lot of people, they are unpaid, you know, workforce who are going to hit — like get hit massively,
economically. They are not sitting at the decision table. If you look at many of the national workforces that are discussing this, you don’t see
that many women.
So, there are very exciting initiative. A group called Women in Global Health, that is a massive global movement, has five recommendations put
forward to the global community to make sure that we have a gender responsive programming.
AMANPOUR: And that’s very, very vital. I want to ask you one last question, because we’re moving to Africa next, and you mentioned how many
of the developing countries are going to be hit much harder by this.
So, Ebola, which we talked about. Did the world learn from the reforms that were made after Ebola? Because that also, eventually, was a joint everyday
by the world that kept — that managed to contain it.
FISSEHA: I absolutely think so. When you see how Ebola was managed between 2014 and 2016, and the most recent Ebola outbreak in DRC, the management
has been completely different. W.H.O. declared emergency — you know, public health emergency very early.
As I said, Dr. Tedros, his personal leadership and that of W.H.O. has been critical. Despite the fact that we had the outbreak that is protracted,
that has been complicated by other outbreaks like measles and what have you in the middle of a warring, you know, faction and war zone, he personally
took about 12 trips to ensure that government was engaged, to ensure that there was political will. That health care providers, front-line health
care providers were getting the support they need. Creating global solidarity. Raising the funds that were needed —
AMANPOUR: OK.
FISSEHA: — to allow the Ministry of Health. So, I think we are improving. It doesn’t mean that we are there. I think we still have a long way to go.
But certainly, his leadership has improved the W.H.O’s response to the global crisis enormously.
AMANPOUR: Thank you very much, Dr. Senait Fisseha, for joining us. Thank you so much indeed.
Now, as we said, Africa is no longer spared the spread of this infection. It has recorded more than 2,400 cases and the W.H.O. says Africa should
wake up.
As we have just been discussing, coronavirus is coming as the last deadly virus to hit Africa appears to be ending. Ebola killed over 2,000 people in
the Democratic Republic of Congo, and that outbreak was the first in the midst of war and doctors trying to combat it also had to face the distrust
of local residents who often believe that Ebola was a foreign plot designed against them.
In an extraordinary film for PBS Frontline, Journalist, Ben Solomon, tells this story through the eyes of three health workers. Now, it’s impossible
to ignore the parallels with today’s pandemic. It’s a tough watch, but we think it’s vital if we want to understand the reality of battling an
infectious disease. Here’s an excerpt from the film.
(BEGIN VIDEO CLIP)
BOSCO KAMBALE SAFARI, MEDICAL TECHNICIAN: My name is Bosco Kambale Safari. I’m a medical technician for dignified and secure burials. Ebola does not
go to a peaceful place, but where there is brutality, the epidemic comes there. Where there is strife, that’s where it takes root. Where there is
pain, that’s where it takes root and grows.
Here there is Ebola and there are people cutting us with machetes. Ebola and bring cut with machetes come together here. But if we don’t eradicate
this epidemic, everyone here will die.
BEN SOLOMON, JOURNALIST AND FILMMAKER, PBS FRONTLINE: One of the world’s deadliest diseases is being fought in one of the world’s most dangerous
regions. Health workers are frequently attacked by Congolese who don’t believe Ebola exists.
UNIDENTIFIED FEMALE: A group stormed into a hospital where an Ebola team was meeting and killed an epidemiologist with the World Health
Organization.
MARIE-ROSELINE DARNYCKA BELIZAIRE, MEDICAL DOCTOR: I am Marie-Roseline Darnycka Belizaire. I am medical doctor. I’m from Haiti. I think this is my
duty to be here in the field. As I chose not to do medicine, I chose to care for people.
But this is the first time that we have Ebola in a war zone. And the biggest problem is, this is a community that doesn’t trust outsiders.
Today, a young boy died. An Ebola body is highly infectious. So, we have to convince the family to let our team make a safe and dignified burial.
We are going to protect the body. You’ll be able to see it. All of you. You’ll see the way we will deal with the body. You’ll be able to check
everything the team will do and supervise your son’s body.
They don’t trust us. They ask us, why are you coming here? And they say, we are in a war zone. We have been killed for so many times. So, why are you
coming now?
I was ready to fight Ebola, but I wasn’t ready to fight against the trauma of this community.
How can we work if we were under attack? I do not understand how people can be so, so, cruel toward us while we are trying to do our best to save them
from a deadly disease. But I am doing what I love. So, if we have to die here, we have to die some days.
UNIDENTIFIED FEMALE: Rumors started swirling that the disease is a hoax, invented by the government and foreigners to control the population.
UNIDENTIFIED FEMALE: Although there’s an Ebola vaccine, responders are struggling to contain the disease.
UNIDENTIFIED FEMALE: The violence has surged. Ebola teams will arrive in a neighborhood to bury a body and people just spontaneously attack.
UNIDENTIFIED MALE: When this thing is the community, it’s possible that it could reach my home. I have seven children. Apart from the Red Cross, I
also sew. My world at the Red Cross, it’s just about helping the community. Because if the disease can get to other children, it can also come to my
home. There is danger here.
UNIDENTIFIED MALE (through translator): This is the corpse of a child.
UNIDENTIFIED MALE (through translator): I feel such pity. Sometimes, I consider maybe giving up.
And I think again and realize that the whole area will die. Even my children will die. No, I have to continue.
I find the courage and keep going.
UNIDENTIFIED FEMALE: Right now, the situation of security is better. If the day is calm, we go to the field. We cannot be only medical here.
UNIDENTIFIED MALE (through translator): Stop touching him first. You refuse to touch your own child.
UNIDENTIFIED FEMALE (through translator): Oh, my God. My child is dead. My child!
UNIDENTIFIED MALE (through translator): Mother, do not touch him.
UNIDENTIFIED FEMALE (through translator): My child.
UNIDENTIFIED MALE (through translator): They always lied to us. There is no Ebola. Now it’s time to EDS. The secure and dignified burial. We put the
corpse in the bag.
If you open the bag, you will be exposed to the virus.
UNIDENTIFIED FEMALE: They don’t want strangers here. But we brought back a survivor to his village.
(APPLAUSE)
UNIDENTIFIED FEMALE (through translator): Today, Ebola is far away from Muhindo . So we also want Ebola to be far away from the whole population.
This is why I’m using the occasion to ask if there is anyone presenting any signs or symptoms in your homes.
If we start the treatment at the beginning of the symptoms, we can also save him that way. We have saved Muhindo today.
UNIDENTIFIED FEMALE: The people that can prove it best that Ebola exists is a survivor.
JOPHET KAMUISA KASERE, Ebola Survivor (through translator): My name is Jophet Kamuisa Kasere. I’m a survivor of Ebola.
My family, who have passed away, they were more important than me. I am nothing. I am alone at home.
I was approached to help the others.
Katembo!
I’m here to help the children whose parents are already sick. Their mothers and fathers are ill. They are at the Ebola treatment center.
Do you want to see your mom?
Really, when I’m with the children, it makes me happy. I’m at peace.
When the parents come out of the Ebola treatment center, you will find that the children tend to want to stay with us, because we regard them as our
own children. In any case, with these children, I am saved.
Yes. Yes.
This is Katembo. His father has died and his mother has fallen sick. Katembo, I consider him like my son. And I forget the past.
One more? You really love rice a lot. Wow.
(LAUGHTER)
UNIDENTIFIED FEMALE: The number of people becoming sick has reduced in other towns and cities like Beni, but doctors are still struggling to
contain the disease in the villages farther out.
World Health Organization officials say they’re hoping to have zero Ebola cases by the end of the year.
UNIDENTIFIED FEMALE: We’re starting to see the change. We have more people trusting the vaccinations. I think the community want to see Ebola ending.
UNIDENTIFIED MALE (through translator): If the population understands, if they respect everything, if they secure the body, and bury it without
problems, it will be eradicated.
But if misinformation is transmitted to people, the epidemic will continue to spread. And as long as people remain stubborn and cause trouble, the
situation will never end.
KASERE (through translator): You hear rumors that there will be an attack at the Ebola treatment center. I tell myself that, if I remain at home,
this child could get hurt.
So, the love we have for these children makes us stay, despite the danger.
UNIDENTIFIED FEMALE: It is chaos here. So now, we are very frustrated to see that all those efforts are reducing to nothing just in one day.
It hurt — it hurt us so much to know that there are some people in need of our help. It hurt even more when we know that those people can be spreading
the disease around them, wiping whole communities, whole families. It’s hurting very much.
(END VIDEOTAPE)
AMANPOUR: Now, on every single level, the Ebola crisis was the canary in the coal mine for what we’re facing with coronavirus.
Now, the world did come together to fight that, and here in this Congo area, there has been no new cases of Ebola since February 17, a really
amazing cause for hope.
And as you saw there, Jophet lost many members of his family, but found some comfort in joining the fight against the disease and caring for other
Ebola orphans.
Grief, as we know, is a natural part of the human condition, and around the world today, people are united in their sadness, as family members and
friends die of coronavirus, sometimes alone in isolation or ICU.
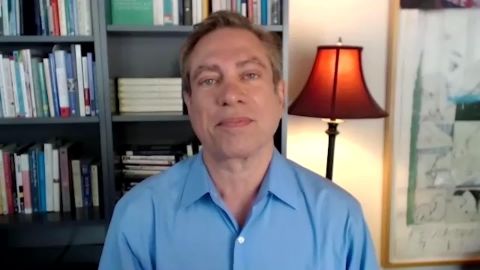
David Kessler is one of the world’s foremost experts on loss and healing. He’s author of “Finding Meaning: The Sixth Stage of Grief.”
And he tells our Michel Martin how we can share our pain across these new boundaries and what he learned from the loss of his own mother and son.
(BEGIN VIDEOTAPE)
MICHEL MARTIN: Mr. Kessler, thank you so much for joining us.
DAVID KESSLER, AUTHOR, “FINDING MEANING: THE SIXTH STAGE OF GRIEF”: Thank you for having me.
MARTIN: I keep hearing anecdotally, and I’m pretty sure if there’s research on this, it would be borne out, but a lot of people are just
feeling something right now.
And you say that what we’re feeling, beyond the discomfort, beyond the inconvenience, you say what we’re feeling is grief. Talk more about that.
Why grief?
KESSLER: It’s interesting.
What I’m hearing from people is, I woke up with this heavy sadness, or I was going to bed with this heavy sadness, or I just feel this heaviness.
And, really, when I hear what they’re saying, they’re describing grief. We are grieving the world we have now lost. Our normal life, our routines,
seeing people, our work, everything has changed.
MARTIN: I take it that a lot of people are uncomfortable with that. They’re uncomfortable with the fact that they feel so disoriented.
Do you agree with me? And, if so, why would that be so? Why would we be so impatient with ourselves that we’re feeling this?
KESSLER: Well, we’re a society that always wants quick fixes. So, we want this to be over quickly.
And this is looking like our world has changed. And I think it’s sinking into us that, next week, the world is not going to go back to normal. In
fact, that normal world is probably gone forever. And change is actually grief. And grief is usually a change we didn’t want.
This is clearly a change we didn’t want, the same way we talk now about, do you remember, before 9/11, what airports were like? I think we’re going to
have discussions about, do you remember what the world was like before the pandemic? Do you remember how we used to shake hands? Do you remember how
we used to do this and that?
I think we’re seeing a loss of our world, and we are feeling the grief that goes along with that.
MARTIN: Is there some benefit, do you think, toward naming it as grief? If we were to all — I’m not quite sure how we would do this, but, as a
society, as a country, just acknowledge that we are all grieving, do you think that would be helpful?
KESSLER: Yes.
And I think there’s something so important. We had to do this with 9/11, but it was a moment that we could see. We don’t even know how long this
moment is going to last.
But I think if we acknowledge, this is grief, this is loss, we haven’t dealt with a lot of people dying yet, and I hope we don’t. My guess is,
that’s coming. But, right now, our world as we knew it has died, and we’re feeling the sadness.
So, if we name it, it allows us to be sad, to cry, to feel those emotions, because, in a strange way, our emotions need motion. We need to feel them.
Suppressing them isn’t going to work. Work.
MARTIN: You have talked about our sense of communal grief, the fact that we’re all experiencing something, and you would like to help us name what
we are experiencing as grief.
But there are some who know that they are grieving, because they have lost someone, they are about to lose someone, someone might be quite ill and is
— they’re unable to visit that person. We know that a lot of facilities, nursing facilities, are in lockdown, for perfectly good reasons.
But do you have some words for people who they’re experiencing kind of a private grief that everyone knows, but they can’t — they can’t address it
in the way that we normally would do?
I mean, what would we normally do? We would take a person food. We would go sit with them. We would visit with them. And, in some cases, this is not
possible.
KESSLER: You’re so right, because grief is about being with someone, not doing them.
And we have to look at it differently to find creative ways. So we are having to say things like, I’m going to the grocery store, I bought some
fruit and some vegetables, and I left it at your door for you. We’re not able to bring the food in, but we still can leave it for people.
As you mentioned, for the first time in our history — we have had so many tragedies, but we never had tragedies that you cannot have a funeral, a
memorial. That is something we have never had to deal with.
So, people have had tremendous losses and are completely isolated. And I’m encouraging people to have virtual funerals, if they need, for now, because
I’m afraid we are going to see a lot of loss. And there is something about a death that it needs to be marked when it happens.
If we’re all brutally sad right now that our aunt has died, this week we should have that virtual funeral. I would never have suggested that in my
life, but that is the world we’re in today.
MARTIN: We have seen that the president in particularly has — seems to enjoy this metaphor of fight. This is an enemy and we’re fighting this
enemy.
What do you think of that?
KESSLER: Well, it is an enemy.
I get concerned that we’re fighting this enemy not medically as much as we should, but more economically. And it is truly a medical fight we are in.
This is 100 percent a medical fight. The economy is the symptom of the problem. You can’t cure anything by being in the symptom. You have to go to
the medical aspects of this. So, that’s my concern around that.
MARTIN: David, I’m asking for a value judgment here, but do you think that, in some way, Americans are in denial about how serious this is, apart
from the politics of it?
Obviously, there are certain people very eager to get people back to and get the economy moving again. But you also see stories about people being
unwilling to upend their rituals, despite pleas to do so.
Do you think that Americans are in denial about how serious this is?
KESSLER: That is my fear.
My fear is very much that we think we have gone through the five stages and we have now got to acceptance and bring our life back. My fear is, we are
still in the first stage, that we are in denial.
And as I talk to people around the country, and they’re like, you’re in lockdown, why would your government do that — and when you talk to people
in Italy or China or other places in the world, they are begging us to take this seriously.
MARTIN: So, let’s talk more about what steps do you think that we could be taking to address our grief.
I mean, I think — what I think I hear you saying is, the first thing is to name it, name it as grief.
KESSLER: Right.
(CROSSTALK)
MARTIN: Now that we have done that, what else?
KESSLER: The next thing to do is to stay in the present moment.
The reason why this is so important is, we have what we call anticipatory grief. That’s the anxiety of the future. We begin to picture everyone we
know sick. We begin to picture people around us possibly dying, and we see a horrible image of the future.
And we have to bring ourselves back into the moment and go, we’re healthy now, we’re safe, we have got enough food, everything’s OK in this moment.
The next tip is to understand what you have control over and what you don’t. And take control over, I can stay six feet from people. I can wash
my hands. I can use sanitizer. I can stay at home, absolutely, unless it’s, you know, very, very essential.
That’s what we can take. If your neighbor isn’t doing it, then you just need to find your control and stay away from your neighbor.
MARTIN: And what about people who don’t have everything that they need, who are genuinely frightened? There are people who are living on fixed
incomes who did not have the opportunity to stock up, as other people with more means may have, people who have lost their income suddenly.
I mean, they have legitimate reasons to be concerned, to be anxious, to be frightened. Do you have some thoughts for them?
KESSLER: This is really a time for us to truly become a community.
You know, my street that I live on, we all for the first time were on a text together. Does anyone have extra toilet paper? Oh, I know there’s an
elderly person in that house. Let’s go knock on their door, and step back six feet, but make sure they have what they need.
This is a moment to truly become our brothers and sisters’ keeper.
I had the privilege of spending time and working with Mother Teresa. And one of the things she was asked once about the poverty in her country, and
she said, you know, sometimes in America, you have a poverty worse than ours.
She said, in our country, if someone has one banana, they share it with everyone. So many people in your country have so many bananas, they won’t
share any of them.
This is a moment for us to share what we have.
MARTIN: I know one of the reasons that you are quite well known around the world is the work you did with Dr. Elisabeth Kubler-Ross, the stages of
grief.
And you have also written about what you call a sixth stage of grief. And forgive me from pointing out that this comes from losses that you have
experienced yourself personally.
KESSLER: Right.
MARTIN: And I’m so sorry for those losses, the loss of your son in particular most recently.
Can you just talk about that?
KESSLER: Sure.
MARTIN: And why is it important to acknowledge what you call the sixth stage of grief?
First of all, what is it, and what role does it play in our lives?
KESSLER: Sure.
The sixth stage, I believe, is meaning. So, many people know Elisabeth Kubler-Ross’ stages that I was privileged to work with her on, denial,
anger, bargaining, depression, and acceptance.
They’re not linear. They’re not five easy steps. Our grief is as unique as our fingerprint. There’s no map for grief. Everyone does it differently.
And Elisabeth would have told you that herself had she been here. And, as you mentioned, my younger son died a few years ago, David. And I found
acceptance wasn’t enough. I needed more.
And that more for me was, how can I make meaning? And so the book is “Finding Meaning: The Sixth Stage of Grief.”
I believe, after this, when this is over, when this subsides, we’re going to go back, and we’re going to look and go, what is the meaning? What can
we learn from that? What post-traumatic growth can we find?
My hope is that we do this in a way, compassionately, lovingly, where we come out with post-traumatic growth and not post-traumatic stress. And that
will be the meaning.
MARTIN: Let me just say — I apologize if this is a sensitive subject, but you’re so generous in sharing your own feelings and experiences with us,
and I appreciate that so much.
You wrote that, when your own son died, that you learned things that you had not known, even though you are an expert in this area. Can you share
what some of those things may have been?
KESSLER: Well, being a grief specialist for decades, I had thought my losses were long behind me.
I had gotten into this work because of my mother dying while there was one of the first mass shootings in the U.S. So, coming from such a traumatic
childhood, I thought, that’s all behind me. There was no part of me that was prepared for my son to die unexpectedly.
And it really reminded me of how painful grief can be. I wanted to write a note to every parent I have ever counseled saying, I had no idea how bad
the pain was.
But I knew, for all of us, we can’t let people die and not find something honorable to bring forth to the future about them. And that was the
meaning.
You know, my son, in kindergarten — and he died at 21 years old — when he was in kindergarten, they gave out little trophies and awards for everyone,
as we do. And he got an award for being the most likely to become a helper.
MARTIN: Hmm.
KESSLER: David never got to become a helper in his life, but in his death now, with the new book and my work, he is helping so many people around the
world he will never get to meet. And that’s my meaning in his honor.
MARTIN: I wonder if you have just some words of — to help us find the compassion that you say we so desperately need, because I do think there
are people who are very — people are still going through all the — they’re going through all the feelings, right?
KESSLER: Right. Right.
MARTIN: People are all different places. They’re angry. They’re angry at other people. They’re angry at the situation. They’re frightened. They’re
all the things.
So, is there a way you can help us?
KESSLER: Yes, to remember the worst loss is yours.
If your teenager is suddenly out of school, that is their worst loss. So, we have to recognize these are losses for each of us.
The other thing, as we judge, our neighbor, our friend or co-worker, to remember, oh, I have made mistakes too.
And the third thing — and this is a really — this really guides my life – – everyone is fighting battles you know nothing about. We get into arguments with people, and, later, we find out their wife was leaving them,
something horrible was happening, they had an ill child.
You don’t see the full picture in anyone, sometimes even our spouses. Everyone is struggling in ways we don’t always understand, so we should try
to be kind.
MARTIN: Well, David Kessler, thanks so much for talking with us.
Before we let you go, how are you doing?
KESSLER: I’m doing all right.
You know, one of the things, that I have received thousands of e-mails from people who can’t go to their in-person grief support groups, or they just
had a loved one die and can’t have a funeral.
So, on Grief.com, people can find a daily free online grief group that I’m doing to make sure people in grief get taken care of during this difficult
time.
MARTIN: Well, thank you for talking to us.
KESSLER: Thank you.
(END VIDEOTAPE)
AMANPOUR: Digging deep to find meaning and kindness.
And, finally, many fantastic odes to spiritual resistance have been posted online, and we want to leave you with Beethoven’s “Ode to Joy.”
Musicians from the Rotterdam Philharmonic in the Netherlands have come together from their homes to reach out to each other and to all of us in
our distance and our isolation.