Read Transcript EXPAND
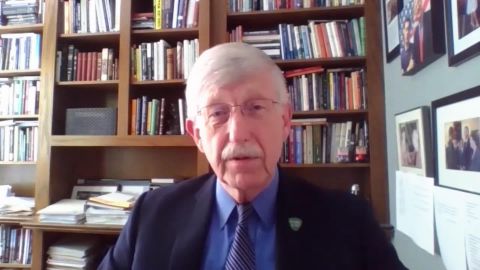
CHRISTIANE AMANPOUR: Our next guest has spent 20 years leading public health research in the United States. Dr. Francis Collins is the director of the National Institutes of Health. And, as such, he is the boss of Anthony Fauci, who’s the nation’s top infectious diseases expert, as you all know. Here is our Walter Isaacson talking to Dr. Collins about which vaccine trials especially excite him right now, and how he’s relying on his faith during this pandemic.
WALTER ISAACSON: Thank you, Christiane. And, Dr. Francis Collins, thanks for all you’re doing for the country, and welcome to the show.
DR. FRANCIS COLLINS, DIRECTOR, NATIONAL INSTITUTES OF HEALTH: Thanks, Walter. It’s great to be with you.
ISAACSON: Let’s talk about Russia, which announced this week that it’s going to roll out a vaccination that has been — passed the safety trials, but hasn’t gone through those phase three trials to see if it works, whether it’s efficient yet. Do you think that’s a good idea?
COLLINS: I think that’s a pretty bad idea. We do phase three trials for two very important reasons. One is to be sure that it really is safe in large numbers of people, that is, to make sure there’s not one in 1, 000 people who has a bad side effect. You wouldn’t know that from the small phase one and two trials. But, secondly and really importantly, you do the phase three trial to see if it really works in the real world. It’s fine to say you have a vaccine that made some antibodies develop, but you want to know whether it prevented disease. There’s no way to do that without doing the hard work of a phase three trial, with tens of thousands of individuals in a community where the virus is actively spreading, and you can see whether it prevented them from getting sick. That’s what we’re doing right now in our vaccine trials in the U.S. And I’m surprised Russia thinks you can skip over that.
ISAACSON: But if the Oxford vaccine, which you have been backing that AstraZeneca is going to do, or the Moderna vaccine, that also have been proven very safe, why, if somebody like myself says, OK, it looks really safe to me, I don’t know fully whether it’s going to work, but I’m willing to try it, wouldn’t that help give you more evidence of if it works? And wouldn’t that be something that I should have the right to do?
COLLINS: I would say, Walter, you should sign up for the trial, where the…
ISAACSON: I want you to know, I have gone to coronaviruspreventionnetwork.org. And I have signed up for the trial.
COLLINS: Excellent.
ISAACSON: But if I don’t get in, I want to know, hey, can I get the vaccine in?
COLLINS: If I were you, I’m not sure I would volunteer out of a trial to learn from the circumstance, because you might be sort of getting yourself injected with something that ultimately turns out not to be very helpful. There is this also unlikely outcome, but we need to watch for it in the large-scale trial, which is called vaccine enhancement of disease. And this has happened with RSV. It’s happened in a couple of instances with rare conditions, but it is unlikely to be the case here. But you want to know, is there any way that the vaccine kind of revs your immune system down the wrong paths, and then, when you encounter the virus, it actually causes more severe illness? I don’t think that’s going to happen here, but we need to know that.
ISAACSON: What do you need to make sure that the clinical trials you’re undergoing are effective and working well?
COLLINS: Well, we need volunteers, and we need a lot of them. In order to really have the appropriate power to determine if the vaccine is working, we need about 30, 000 people. Half of them will get the vaccine. Half will get a dummy placebo. You won’t be able to tell which one you got, and the people administering to you won’t know either, because that’s the way we make sure that we can really determine what the vaccine did. But it will be particularly important that the people who volunteer represent the groups who have been hardest hit with this illness, and that means older people, people with chronic illnesses, African-Americans, Latinx, because we really want to understand how the vaccine performs in a circumstance where it’s going to matter the most, which is to protect those vulnerable people from illness.
ISAACSON: One of the other vaccines that you’re backing at the NIH is from Moderna. And it uses an entirely new type of process, which is to not put it — to send in messenger RNA. That’s a totally untried, new method, isn’t it?
COLLINS: It has never been used to develop a vaccine that’s gone all the way to FDA licensure, but it is a very appealing approach, because you can build the vaccine so quickly. When the sequence of the viral genome from coronavirus was released by Chinese scientists in mid-January, the design of that Moderna vaccine at our own research center at the NIH took place in about a day-and-a-half. And just 63 days later, that first phase one trial got under way, where people were being injected with that mRNA, which basically codes for the same thing. It codes for these proteins. But you stick the RNA into a muscle, and then the muscle goes, oh, this is RNA, I know what to do with this. It makes the protein for you. And then the immune system sees it. So, it’s quick, it’s elegant. And we shall see whether it’s actually going to be successful. We will find that out in a few months. By the way, I should say, there’s another vaccine very similar to that that’s being put forward by Pfizer which is also now in phase three trials using the mRNA approach.
ISAACSON: So these are in phase three trials. When do you think we’re going to at least start to get information about whether they’re efficient?
COLLINS: Well, a lot will depend on how quickly we can enroll, because we really think we’re going to need tens of thousands of people for each of these vaccines, and there are several of them. So, you add it up, we’re talking about more than 100, 000 people that we hope will take part. These vaccines, for the most part, are two doses. So, you get a dose on day one. And then, 28 days later, you get a second dose. And then we start watching to see what happens after that over the course of the next one or two months to see whether people in fact do still fall ill. If you got the vaccine, and then you got sick anyway, that’s not a good sign. If you got the placebo and you got sick, but the vaccine people didn’t, that would say, looks like it’s working. So, all of this will have to play out over the course of two or three months. I think we got to be careful not to make wild claims about how early we would actually get a signal here. There will be a group that’s unblinded to the data that will be looking all along the way on the chance that, A, there’s a safety signal we need to know about, or, B, it looks like it’s working even sooner than expected. But, mostly, I would guess we will not have an answer until pretty near the end of this year about whether one or more of these vaccines is actually safe and effective.
ISAACSON: So, if they start detecting that some of these vaccines may be working well, say, in October, November, might you say, OK, let’s just give it emergency authorization, get it out there?
COLLINS: I don’t want to think that the FDA would do that, unless the data was really compelling. The worst thing we could do would be to prematurely declare victory, when we don’t have the evidence to do so. And Steve Hahn, who’s the commissioner of the FDA, has made it very clear that he will not be granting any emergency use authorization, unless the data is compelling, that it’s safe, and it’s at least 50 percent effective. And, ideally, it should be higher than that. So, yes, we will have to wait until we reach that threshold. Otherwise, it’s still an experiment.
ISAACSON: How optimistic are you that we’re getting more treatments online now?
COLLINS: We have some real progress to report. And a lot of that is because of a public-private partnership called ACTIV, which stands for Accelerating COVID-19 Therapeutic Interventions and Vaccines. We do, after all, know that remdesivir, an antiviral, does have benefit for people who are sick with COVID-19 in the hospital. We know that dexamethasone, a steroid, reduces death rates, particularly for the sickest patients who are in ICUs or on ventilators. But we have a bunch of other things that are coming along. There are high hopes that convalescent plasma, where you get a plasma donation from somebody who has survived COVID-19, and infuse that into somebody who’s just gotten the illness, you might speed up their recovery by giving them those antibodies they haven’t quite made yet themselves. There are hopes that that will be beneficial. We don’t quite have the evidence to be compelling about that, but we’re working hard on it. Then right on the heels of that would be something that I am pretty excited about, which is monoclonal antibodies, where, again, you start with somebody who has survived COVID-19, you identify very powerful antibodies that some of them have that bind tightly to the virus, so-called neutralizing antibodies. And then, using biotechnology, you purify those and make them in large, pure quantities as a drug. And those trials are about to start for both inpatients and outpatients.
ISAACSON: I guess one of the big questions we all have is about schools and reopening. In the past week, we have had the Centers for Disease Control talk about that Georgia summer camp. We have had a few test cases of schools reopening. How optimistic are you? And what should schools be doing?
COLLINS: This is going to be so much dependent upon local conditions. If I were a school board president or a principal trying to sort that out, I’d want to look and see, what is the spread of this virus in my community? And there are all kinds of metrics you could use. One of the ones that’s turning out to be most useful is looking at people who are getting tested, and say, what percentage of them are positive? I mean, think about that. If you have people being tested, and only one 1 percent are positive, that means there’s not a lot of virus out there. If it’s 15 percent, like it is right now in Florida, that says you have got a really serious problem. The virus is traveling around in a pretty unabated way. And that might not be the moment to bring people back together in school, particularly as you think about the teachers and the risks they may be put at. And there have been suggestions that maybe younger kids don’t get infected and don’t pass this on. I think the data to support that optimistic view is looking a little shaky, especially after, as you just mentioned, this report about the outbreak in the Georgia camp where kids of all ages clearly got infected and clearly transmitted it. So, those things all have to be put into the decision-making for a particular school district to decide what to do.
ISAACSON: Why did testing get so bad and so difficult? It now takes a week here in Louisiana, in New Orleans, to get results back.
COLLINS: We do have a serious testing issue right now with the slow turnaround. The good news is, we’re doing a lot of testing; 60 million tests now have been in the U.S., which is more than anyplace else. The problem is, the turnaround has really gotten backed up, as the central laboratories that are doing a lot of this. And main laboratories run by companies like Quest and LabCorp have just gotten really backed up with demands and there are problems with the supply chain and things like swabs and reagents. So, what we really need now, Walter, is to have more diversity of testing opportunities, and particularly the kinds of tests that can be done at what you call the point of care, where you don’t have to get the sample and then ship it off somewhere, but you can get the answer right away in 30 minutes or less. Last Friday, we announced awards to no less than seven companies, mostly small businesses, that have some very inventive approaches to doing viral testing that are ready for a big scale-up opportunity. And we are putting $250 million into that to try to get those out there as early as September, so that we could have more ways for testing to happen, particularly in high-risk situations like nursing homes or meatpacking plants or schools or child care centers, where you could get the answer right away. If you had a nursing home, where the staff walks in, and they get tests before they even go see the first patient, and, if they’re positive, they get sent home, we might be in a much better place than we are right now.
ISAACSON: Why has coronavirus roared back in the United States more than in Europe or elsewhere?
COLLINS: Well, the sad truth is, we never really drove the virus down to the baseline, the way many countries in Europe did after their very serious outbreaks. Basically, we didn’t really follow the CDC’s rules about how to open up carefully. And people were tired of all the things they were asked to do. And leaders of various states and principalities kind of jumped over steps that were supposed to be taken more carefully following the metrics. And now we are in a tough spot. Debbie Birx said, we are looking right now at really quite a worrisome situation, where this virus is kind of the monster that’s all over our country. It’s in cities, but it’s also in rural areas. And we are going to have a very tough several months ahead. And our best antidote for that, which just seems so obvious, and also seems so frustrating and boring, is to do those things that we should have been doing more carefully, wear your mask as soon as you leave the house, don’t congregate, and certainly not in indoor spaces, where you’re crowded all together. Maintain that six-foot distance. Wash your hands. Everybody has to take responsibility. If you’re not worried about yourself, at least worry about those that you may infect, if you become the person who transmit to the older person down the street or your grandparents. This has to be something we all wrap our arms around and say, we’re going to do this. Just like wearing seat belts, it’s good public health. And we can’t afford to say we’re tired of it, because the virus doesn’t care if you’re tired of it.
ISAACSON: Why do you think so many things about this disease, especially the wearing of masks, but even hydroxychloroquine use or whatever, has become partisan and politicized? Is that some lack of respect for science? Or is it just the hyper partisan nature of our society?
COLLINS: Our society certainly is hyperpartisan. Tony Fauci, who is my wonderful director of infectious disease at NIH, and obviously a very visible spokesperson for what we all need to do together, we meet every evening by phone just to see what’s going on, and often commiserate about, how is it that we got into such an unfortunate situation, where something that should be completely nonpolitical somehow has become so? I think it is a reflection of the fact that, in our country right now, everything is partisan, everything is polarized. That’s sort of the default. And it doesn’t take much of a tip of the balance one way or the other for people to decide, OK, I have got to add that to my particular collection of behaviors that define who I am in terms of my politics. This never should have been there. But, unfortunately, it got there. I will hope we can extricate it and decide at this point, with the president himself now telling people to wear masks, let’s all do it. And let’s not pretend that we’re somehow exempt because of where we live or what other kind of aspect of our behavior might be protective. I have got to say, I’m a person of faith. And it’s troubled me also to see that, in some instances, faith traditions are getting on the wrong side of this by suggesting that it’s really not appropriate for churches to worry about these things. After all, that’s God’s house. Well, yes, they are God’s house, but God probably also gave us the opportunity, through science, to learn what is good and safe. And we’re expected, I think, to pay attention to that if we’re going to be reasonable children of the God’s — the God’s creation. So, when somebody said to me, as they did a little while ago, I’m not going to wear a mask in my church, Jesus is my vaccine, I was thinking, where have we come to that we have somehow gotten this mixed up? So — and the conspiracy theories, of course, don’t help either. That’s another big part.
ISAACSON: You wrote a beautiful book called “The Language of God.” It was about your Christianity, your faith. As you talk to these religious communities and people of faith, how is your ability to talk to them better because you are such a person of faith?
COLLINS: Well, I don’t know if it’s better, but I do feel a great relationship and warmth to my brothers and sisters who are people of faith and who are going through terrible struggles, and most of them doing so with great sense of calling to try to do what they can, not necessarily focusing on, why did this happen, but on, what can I do? And you can see that happening running food banks, and making masks for people, or figuring out a way to go to the grocery store for an elderly person down the street, so that they don’t have to take risks. The church is often called upon at times of crisis, and they are responding. But there’s this fringe there that sometimes seems to have aligned itself in a fashion that’s more political than spiritual. And that hasn’t necessarily turned out all that well. I guess, again, as a person of faith, if I have the chance to speak to people in that place, and ask them really to think carefully about what these messages are, and how we are all called upon not to put others at risk, it does seem like that falls particularly on the shoulders of people of faith, who have always defined themselves by taking care of those who are vulnerable and less fortunate.
ISAACSON: And how does your faith help you cope with the day-to-day challenges and horrors that you face with this disease?
COLLINS: I will be honest that seeing the suffering and death around us from this pandemic, I am not immune from wondering, why would a loving God allow such a thing to happen? And yet, at the same time, scientifically, I know exactly what seems to have happened here, that a virus that was previously living in a bat found its way into humans. And I can’t really expect God to jump in supernaturally and prevent that. That’s part of the nature of things. So, I guess, in that regard, I think we are called upon, as believers, always to look at circumstances like this, try to understand what we can do. Tom Wright, in a wonderful essay for “TIME” magazine, points out that we’re also-called just to lament and to feel this burden of sorrow for the way in which things are not perfect. But I also lean upon some of those things that lift me up. Psalm 46 is a particular favorite. “God is our refuge and strength, an ever-present help in trouble.” OK, we got trouble here, and we have got an ever-present help. And I’m going to hang on to that.
ISAACSON: Dr. Francis Collins, thank you so much for being with us.
COLLINS: Walter, it’s great to have this conversation with you. We covered a lot of ground.
About This Episode EXPAND
A special report for Beirut, Lebanon. Then, Christiane speaks with the superintendent of a Mississippi school district, former Secretary of Education Arne Duncan, and soccer icon Megan Rapinoe. Walter Isaacson speaks with NIH Director Dr. Francis Collins.
LEARN MORE