Read Transcript EXPAND
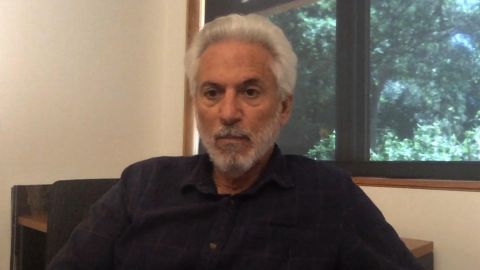
CHRISTIANE AMANPOUR: Our next guest, Dr. Richard Levitan, has been practicing emergency medicine for three decades. When the virus began to overwhelm New York City at the end of March, he rushed from his home in New Hampshire to volunteer at Bellevue Hospital, where he trained in New York. And he speaks now with our Hari Sreenivasan.
(BEGIN VIDEOTAPE)
HARI SREENIVASAN: Dr. Levitan, you have been an E.R. doc for 30 years. You specialize in airways. You decide, in this crisis, to volunteer at the hospital that you`re trained at. How do we keep people from having to be on a ventilator?
DR. RICHARD LEVITAN, EMERGENCY PHYSICIAN, LITTLETON REGIONAL HEALTHCARE: This is a respiratory virus. It gets into the lungs, and over the period of several days, it causes collapse of the air sacs in the lungs. And as the oxygen goes slowly down, the patients just accommodate. They accommodate by breathing a little bit faster, but they don`t realize that. It is remarkable, throughout medicine, how we see that disease processes that come on slowly are well tolerated by patients. So, what is amazing about this disease is the onset of this pneumonia takes days. And, as that happens, patients don`t feel short of breath. But our public health message has been, don`t go to the hospital unless you`re short of breath. So this disease is remarkable in two respects. Number one, a huge number of patients hit the health care system all at once. And that`s just the nature of a pandemic. But, number two, they all presented with advanced disease. And what I`m saying is that, as we have learned more about this, I believe we can change that presentation window from one of advanced disease to more milder and even very mild disease, and that that is an enormous win for the patients and for the system.
SREENIVASAN: You`re saying that our messaging has been inaccurate, at least based on what we knew when we knew it, because by the time someone is coming to the hospital short of breath, it might already be too late to help them.
LEVITAN: I don`t think the word too late is the word to use. I think that, by the time they are coming to the hospital with subjective shortness of breath, their pneumonia is very advanced. But what we have learned in New York just over the last month — and I say we — the credit goes to the front-line health care workers who are overwhelmed in Queens and Brooklyn and the Bronx, who realized some very simple things could avoid ventilators, simple things like putting nasal cannula oxygen at high flows onto people, turning them on to their abdomen, so laying on their stomach, that that would boost their oxygen, decrease the work of breathing. And what we found over — and there`s just a recent study published about this. I was the last author. But a fellow by the name of Nick Caputo in the Bronx was the primary author, and Reuben Strayer, who is in Brooklyn, was also on this paper. And what we found was, two out of three patients, even with moderate to advanced pneumonia, were able to avoid a ventilator during their hospitalization. So, I don`t want to tell people that coming to the hospital means you`re too late. But what I am saying is that, if we move, if we change the public education, if we change the messaging, and if we can detect this silently occurring low oxygen level, that we can do so much better for these patients, and I believe we`re going to avoid even more ventilators going forward.
SREENIVASAN: Help explain why it`s so important to keep people off ventilators in the first place.
LEVITAN: So, in many lung diseases, if we bridge somebody who is having respiratory problems, their body will recover, and they only need it for a few days. And we have learned how to do that in a way not to harm them. But in this disease, it seems that putting people on ventilators triggers a cascade of other problems. Like I said, we can fix the lung stuff, at least by numbers, right away, but the subsequent problems of blood clot, of renal failure, of other issues, and the fact that they require to be on a vent for so long is really just overwhelming the system from a resource perspective. So, just to explain, you get a breathing tube, you also get a tube in your stomach, you get a tube in your bladder, you get a central line, a venous line, you get an arterial line. You then need a team of people to move you twice a day. And you need sedatives, a lot of sedatives. Most of these patients require two and three sedatives, and then another medicine for their blood pressure. So, most of these patients are on four I.V. pumps, all of these tubes, all of these lines, they`re not moving, and — because they`re so sedated. Otherwise, they would buck the vent. And they have to be flipped twice a day. You compare that to a patient who has one I.V. line, monitoring, getting oxygen, who`s awake, who`s turning themselves in different positions, so they open up areas of their lung, proning, and these patient-positioning maneuvers, the resource utilization there is a fraction of the resource utilization that is happening in the ventilated ICU patients.
SREENIVASAN: What are the CDC guidelines on when you should go to the hospital? And you`re proposing a different view.
LEVITAN: I am proposing a radically different view. And where I live in rural New England, I drive about 15 miles to a convenience store. And on the front door of my 7/Eleven is the sign. And it says, you`re not going to feel well with COVID. You may have fevers. You may have muscle aches. You may have stomach aches. You`re not going to feel well, but don`t go to the emergency department. What they`re telling people is, go to the emergency department if your fingers or your lips turn blue. And what I`m saying is, I think, if we move this window of presentation, if we educate patients to come in earlier, if we can do point-of-care testing in the E.R., and know, OK, you have COVID, and then we monitor their oxygen, we can make a dramatic difference.
SREENIVASAN: Doctor, one of the things, though, people are concerned about is, if they weren`t sick already, that going to the E.R., they`re definitely going to be sick, because that`s where all the sick people are, right? There`s still this hesitation about having to go to a place full of sick people to be tested, diagnosed or treated.
LEVITAN: So, late last night, I got an e-mail from an emergency physician in Northern Italy. And he explained to me, we are seeing earlier cases of illness, and we`re doing much better. And so I immediately asked him, so, why is that? He says, well, the patients are no longer scared to come in. And so they diagnosed 250 patients with COVID in the emergency department. They sent every one of them home with a tiny little device, a portable, just consumer-grade pulse oximeter. So they sent people home with this tiny little device. One out 20, 5 percent, came back as their oxygen levels started to go down, and they were hospitalized and treated. None of those 250 patients died. If we move this whole management of this disease to earlier identification of who has it, better pulse oximetry monitoring in COVID-positive patients, as well as those at greatest risk for serious illness, I think we can dramatically influence how this country faces this problem, how we deal with it economically, how we deal with it just societally and globally.
SREENIVASAN: You`re advocating for the use of a pulse oximeter almost like a thermometer that we have at home.
LEVITAN: Yes, I think we would do much better as a country if, in the medicine cabinet of every American was a pulse oximeter and a thermometer. And, ideally, a phone call away is the physician who you can talk to about how you`re feeling and, hey, these are my numbers. If you are extraordinarily wealthy, and you have a concierge physician, this is not a radical concept. This is being done. This has been done with all of these people. And people say, well, that`s going to cause a rush on these, and you`re going to — it`s going to cause a shortage. Well, in the hospital, we use a different one. In the hospital, what we`re using the hospital-grade. But I don`t control the supply of these devices. People on Twitter have said to me, oh, the people who need them aren`t going to get them. Well, I don`t control the world supply. But if I did, what I would say is, overnight, tomorrow, let`s make sure that every assisted living community, every nursing home is checking the elderly with pulse oximetry early and continuously. If we did that, we would identify the elderly, who can`t communicate with us often as well with what`s going on with them. So, if we first did all of the elderly, and then we did every COVID-positive patient with pulse oximetry, I think we would have a dramatic impact on this disease.
SREENIVASAN: What do we know about the pneumonia that`s presenting here vs. what the influenza does to a body?
LEVITAN: Well, so, influenza obviously can cause pneumonia, and it can cause death. The reason why this virus is honestly so scary to many is because a lot of the advance — the pneumonia silently advances. So, the human body does not have a lot of responses to low oxygen. It basically has one response initially, which is, you breathe faster. And we know that, among pilots, if the oxygen levels drop quickly, pilots pass out. But we have also learned, with climbers, that if you slowly go up to altitude, and the oxygen is diminishing rapidly as you climb, as you get to 15,000 to 20,000 feet on the summit of Everest, the oxygen level is one- third that it is on sea level. But the human body can adapt. So what we`re seeing with this disease is, oxygen levels and blood gases that I have measured in patients that rival the summit of Everest, and yet the patient is sitting there on their cell phone. And there are other reasons why this is so different than every pneumonia. Most pneumonias cause a problem with both oxygen and carbon dioxide. And when you acutely drop oxygen, you pass out. So, choking, drowning other acute problems that hit the lungs, if you don`t get enough oxygen to your brain, you pass out or you seize. When your lungs don`t work and they get stiff, carbon dioxide builds up, and that has a narcotic effect. So, patients become somnolent. So, clinicians worldwide are looking at patients who have X-rays that look as bad as anything they have ever seen, with oxygen levels that are basically seemingly incompatible with life, and yet these people are on their cell phones. And what happened early in this pandemic is the belief that, well, they`re about to die, let`s put them on a ventilator. And what we realized, and in hindsight is now better understood, they got there slowly. We can correct their oxygenation. And if we keep careful monitoring on them, and decrease the work of breathing, improve their oxygen and keep them off the vent, it`s actually better.
SREENIVASAN: In the midst of this, there are still — there are doctors in California who say, you know what, this is similar to influenza. We have to start the economy back. We have to get people going. Are they wrong?
LEVITAN: So, clearly, we cannot stay hunkered down in our homes for the next three years. I`m not saying that. And I leave to the public health and epidemiology people this — how do we track — and this whole complicated and political question, frankly, about reopening way above my pay grade. But this disease is deadly. It is way more deadly than influenza. And just by the numbers, you look at the excessive death rates all around the world, this is not influenza. And the resources that this disease is demanding from our health care system is influenza times 24 or times 50. The average length of stay of these COVID pneumonia patients who get intubated, they`re staying in the hospital, on average, 30 days. They are requiring to be ventilated for approximately 20 days. That is just incredible, like, from a resource perspective. So, to compare this to influenza is not correct in terms of what it is doing ,in terms of demand, what it is doing to — crushing the health care system. My little hospital up here in Northern New Hampshire is used — is losing $4 million a month because we`re not doing all the elective stuff because of all the outpatient stuff. Every tiny hospital across this country, of which there are 1,500 of them, are basically facing financial ruin. The cost of this disease is being measured in the hundreds of billions of dollars. Each one of these ventilated patients, I believe, is probably costing more than $1 million. So, to say that this is like influenza, I think, is not appropriate.
SREENIVASAN: We have also seen, in the last few days, more research going into blood clotting, something that`s happening in younger patients. I mean, are we discovering this partly because some of those patients are able to get into the system faster?
LEVITAN: Yes, so this disease is complicated. And as we are encountering hundreds of thousands of patients, we`re finding things that this virus does to them. So there are cases of brain infection, encephalitis, this terrible story of this young girl who died. There are cases of the virus affecting the heart, causing myocarditis. We are seeing neurologic complications of this disease. But the overwhelming number of people who die of this disease die of pneumonia. But when you look at this disease, 35 percent, roughly one in three patients who are on a ventilator develop blood clots. The number of people who are not on ventilators and develop blood clots is one-tenth of that. So, what we are learning about this disease is that we can actually address the lungs early on. Whether you get on a ventilator or you don`t, we can fix oxygen, we can fix the lungs. But what happens on the ventilator over time is multi-organ failure. One out of six patients on ventilators will require dialysis. One out of three develop blood clots. So this is an awful disease. And at the end of it, there are many, many complications that spread throughout the entire body.
SREENIVASAN: Do you think that we, as a society, as a health care system, have the potential, so that if or when there is a second wave this fall, that we can deal with this better?
LEVITAN: I don`t think we have a choice. I don`t think we have a choice. I don`t believe this war is going to be won through some magic bullet of a vaccine that somehow we`re going to get to a billion people on the planet. I don`t think we`re going to come up with a single pill that is going to prevent this from infecting everybody on the planet. It would be great if we did. That would be wonderful. I would be happy as heck. But I think that what we need to prepare for is a long, slow battle over 12 to 24 months, but that, through incremental gains, we are actually having a tremendous effect. And what the public needs to know is that we`re learning how to do better with this, simple maneuvers, turning people on their stomach, improving oxygenation, and avoidance of ventilators in two out of three patients is the savings of — I mean, it`s incalculable. It`s billions and billions of dollars, and it`s tens of thousands of lives that will be saved. You know, so, yes, I think the public needs to know that this isn`t an option. Like, for the foreseeable future, until a magic bullet comes along, we need to continue doing these slow, incremental gains. But the public, I think, has not heard this message that we`re getting better. In the ICU, the ICU doctors are learning how to better ventilate these patients, so they`re getting more people off of ventilators who they put on them. So there are lots of wins happening. But the public has this perception it`s all doom and gloom. And I want to tell them that it`s not, that clinicians on the front lines, both in New York and Italy, are reaching out to me and telling me that we`re doing better. And that`s a message of hope.
SREENIVASAN: Dr. Richard Levitan, thanks so much for joining us.
LEVITAN: Thank you very much for having me. Again, I went to New York for 10 days. The heroes in this story are the front-line workers in New York City.
About This Episode EXPAND
The president of Americans for Prosperity joins Christiane Amanpour to answer the question on everyone’s mind: How can the American economy be opened up safely? Then, journalist Michael Specter discusses Anthony Fauci’s career and leadership during the COVID-19 pandemic. Finally, Dr. Richard Levitan joins Hari Sreenivasan to explain why COVID-19 patients should be going to hospitals sooner.
LEARN MORE