Dr. George Daley Extended Interview
It’s been one year since President Barack Obama lifted the Bush era’s eight-year ban on federal funding for embryonic stem cell research. Read excerpts from producer Susan Goldstein’s and correspondent Betty Rollin’s recent interview about ethical guidelines, current research, and the limitations of Obama’s policy with Dr. George Daley of Children’s Hospital Boston, where a new web site is now available on the state of stem cell research.
 Stem cells are the master cells of the human body. They are the seeds for our tissues. They come in two varieties. They are pluripotent, which means they can make any tissue in the body, and the classical pluripotent stem cell is the embryonic stem cell which comes from the earliest human embryos. There are also stem cells in our adult tissues, so called adult stem cells, or better somatic stem cells, stem cells of the body, and I think the analogy to plants is a good one. We are talking about the seeds for our tissues, so if our skin is like a lawn of grass, the stem cells of the skin are the grass seeds.
Stem cells are the master cells of the human body. They are the seeds for our tissues. They come in two varieties. They are pluripotent, which means they can make any tissue in the body, and the classical pluripotent stem cell is the embryonic stem cell which comes from the earliest human embryos. There are also stem cells in our adult tissues, so called adult stem cells, or better somatic stem cells, stem cells of the body, and I think the analogy to plants is a good one. We are talking about the seeds for our tissues, so if our skin is like a lawn of grass, the stem cells of the skin are the grass seeds.
Embryonic or pluripotent stem cells are different from adult stem cells. They teach us different things. If we want to understand the earliest stages of human development, how we lay down all the different tissues, then we are best to study these early embryonic or pluripotent stem cells. If we are just interested in the skin, for instance, then we study the skin stem cell. So it’s not one is better than the other, it’s that they teach us very different things. My laboratory studies both side by side. We study embryonic stem cells as well as the adult stem cell for the blood-forming system, so called hematopoietic stem cells. We found that actually studying both types side by side gives us a much greater insight into their functions.
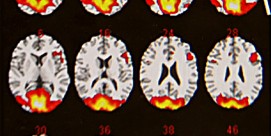
The research is answering very fundamental questions, first of all, but the promise is that one day we might learn to deliver stem cells as curative therapies. For now we can use stem cells to treat diseases of the blood. So if a child has a genetic disease or leukemia or lymphoma, we might use a blood stem cell typically taken from a healthy sibling to try to cure that child’s disease. But there are many diseases that we can’t approach yet with stem cells, other diseases of the blood that aren’t easily treated by bone marrow transplant, diseases of other organ systems like diabetes, or even in adults diseases of the degenerating brain. We believe that stem cells offer a new approach. It gives us a new way of organizing our thinking about the way tissues form and the way tissues could be affected by disease. Stem cells are part of what we call regenerative medicine, because stem cells are involved in the natural repair and regeneration of our tissues. They teach us enormous amount about the disease process, but they give us this possibility for regenerating tissues, and that’s why they are of such tremendous scientific importance, but also potential medical value in the future.
Under the last administration we were operating under a very restrictive policy, so in 2001 President Bush allowed funding for a very small number of embryonic stem cell lines, and over the last decade over 1,000 new lines have been created. The new Obama policy opens up the possibility for federally funded researchers to use all of those lines. So you can imagine it creates a much greater opportunity for scientists to use the many hundreds of lines that have been generated that model specific human diseases, lines that have been made under pristine medical conditions. Those are all valuable, but until the new policy they haven’t been accessible to us who are working under federal funding.
With many governmental policies, the devil is in the details. So the [Obama] policy was announced in March of 2009. In July of 2009, the National Institutes of Health implemented the policy with a very exhaustive new set of guidelines, and in December they’ve approved their first 13 lines. Now our lines from Children’s Hospital were 11 of the first 13, which is very exciting. But now it’s a complicated policy. We have only one line that we were able to use under the old policy that’s been accepted under the new policy, and there’s a pipeline of hundreds of lines waiting for approval. So the policy is in place, but it’s going to take months, maybe a year of more, to implement it. So there’s still a certain delay and frustration.
Embryonic stem cells come from human embryos left over from in vitro fertilization (IVF). One in six couples in our society can’t have children. They are infertile, and they will often turn to in vitro reproductive assistance in a very sincere desire to have their own family. So the egg and the sperm can be brought together in a petri dish. Now in order to make it safer for the woman, this is done in a way that many embryos are created and then frozen away. Then the couple may choose to have one, two, and sometimes three children, and the remaining embryos are left behind. In the past, couples had the chance to discard those as medical waste or to donate them to research, and some chose to donate them for the creation of these embryonic stem cell lines. Now a small number of these embryos can be adopted by other couples, but we are talking about hundreds of thousands of embryos throughout the country, and they are never going to become babies. Now there is an ethical debate about the value, and it essentially pits the societal interest in directing research in the cure of diseases against the moral status of this early human embryo.
Human embryonic stem cells are derived from this earliest stage of human development. Now we are talking about the first three or four days after conception, when the human embryo is a tiny ball of cells, between 50 and 200 cells. It’s a speck smaller than a period at the end of a sentence. You need a microscope to see it. There’s no structure, there’s no body parts. In fact, there’s not even a single cell there that persists in our bodies. They’re stem cells that will give rise to all the tissues. There’s no nerve cells, there’s no blood cells, and it’s a very, very primitive structure that in more than half the cases doesn’t even implant productively in the uterus. So scientists look upon these as extremely valuable cells, tissues, not as people. But the debate rages on because there are some in our society who want to say that the human person begins at the point of conception and therefore should be free from experimentation. This particular view, that life begins at conception, is a historical feature that can be traced to Pope Pius IX in the late 1800s. There are certain other religious groups, evangelical Christians, that tend to hold to this very, very strict notion, life begins at conception. From a scientific point of view I find this curious, because life is everlasting. All cells are alive. The sperm is a live cell, the egg is a live cell. All life has to derive from preexisting life, and then, of course,the life of a cell is very different from the life of a person. When I’m a physician thinking about a patient’s death I don’t think about their cells dying. I think about their coordinated, integrated physiologies stopping. Their brain dies, their heart stops. We define brain death as a way independent of the death of a body. In fact, the body can be sustained in brain dead individuals on a respirator to help with breathing, make sure that the heart continues to pump. This is a very different concept than saying that a cell is alive. But one looks at it from a practical point of view. One actually dissects the very nature of cells relative to the nature and needs of human beings, of persons, persons with disease, persons with needs that call on us in a much greater sense than cells would call on us. I think that we can make those distinctions.
We do believe that there is medical value in creating cells, sometimes in the form of embryos that are matched to individuals. That gives us an enormous ability to take a person’s cells and make them into a stem cell. Now it’s been disparaged as somehow creating human life. The fact is, once again, the cells are all living. We are simply changing the nature of one cell into another for research purposes. Some of the heat around this debate of creating life has really dissipated because of this new way of making pluripotent stem cells which we call now induced pluripotency. So I can now start with skin cells or blood cells and add a few genes. These are genes that are resident in embryonic stem cells that give them this special ability to make any tissue. By simply transferring those genes from embryonic stem cells into skin tissue or blood tissue, we turn them back into their embryonic state. This gives us the opportunity to make stem cells from any patient That way we can study their disease, and we can make cells that are the patient’s own cells so they would not be rejected, should we would want to or need to transplant them back for a type of therapy. It does address some of the ethical challenges, and it gives us enormous new opportunities to study research tools and to develop new therapies.
We need both embryonic as well as adult stem cells in research. Embryonic stem cells and this new form of induced pluripotent stem cells do more things. There are much more basic, fundamental cells. They haven’t become patterned or specialized in any particular tissue. The stem cells from adult tissues are already kind of restricted. The stem cells from the blood only form blood; they don’t form skin.
When President Bush announced his policy in 2001, it essentially took the federal government out of the oversight of most embryonic stem cell research. That left it up to the scientists to create guidelines themselves. Here in the US, the National Academy of Scientists came out with a set of guidelines, and internationally the International Society for Stem Cell Research came out with independent guidelines. I chaired the task force for this international society, and we established guidelines which defined areas of permissible research and impermissible research. There has been a longstanding tradition that respects the ability to work with a human embryo up to 14 days. Fourteen days is considered the time when the early human form starts to take shape, and there’s the sense that beyond that there’s a boundary, and scientists have been comfortable working in the petri dish with the cells prior to that stage. Virtually all international societies that have looked at this respected that 14-day rule.
The most important, fundamental aspect of stem cell research in the ethical guidelines is that the individuals involved be allowed to engage voluntarily with full, informed consent. So the couples that are involved are given tremendous instruction about the nature of stem cell research and the way their cells will be used, and they have the voluntary right to engage or to refuse without it influencing the type of medical care they are going to get. There are those kinds of practices of personal autonomy, voluntary informed consent, the notion that there are permissible and impermissible areas of research, such as a prohibition against human cloning. That’s part of all the ethical guidelines. These are the kinds of principles that have given the scientific community a road map to work from and I think gives the greater community the sense that this is being done with really scrupulous ethical oversight.
We add genes from embryonic stem cells into skin cells or to blood cells, and they become essentially just like embryonic stem cells. So they allow us to model diseases, determine disease mechanisms, understand pathology, maybe develop drugs to repair the pathology, and maybe develop tissues that we can transplant to cure disease. The question often arises, why do we still need embryonic stem cells? We wouldn’t have induced pluripotent stem (IPS) cells without embryonic stem cells. The IPS cells, as they are called, are built on the foundation of knowledge from embryonic stem cells. We are now just learning about IPS cells. They are new. We don’t know for a fact that they are identical to embryonic stem cells. There’s an emerging sense that their genomes may be unstable, that they may have differences that would preclude them from certain clinical applications. So it’s still valuable to understand the natural embryonic stem cells side by side with the IPS cell. There are also many questions, we should remember, that pertain to the earliest human embryos that will never be studied or understood by looking at skin cells that would be turned back into embryonic stem cells. The science of the early embryo is going to teach us things about human infertility, about early birth defects, and unfortunately under the current federal policy we still can’t use federal dollars to study early embryos, and that leaves us ignorant about many fundamental questions, and I think that’s unfortunate. We can study the cells that come from embryos, but we can’t study the embryos themselves by using federal dollars. That is still restricted. So it’s important for people to realize that the Obama policy has opened up new frontiers, but there are still areas that remain closed to federally funded researchers.
There is a deep divide in the Congress that reflects a divide in the US population about the nature of the human embryo. Currently, there is something called the Dickey-Wicker amendment, which is a rider on the appropriations bill that gets renewed every year, that prohibits the use of any federal dollars to be spent on research that destroys an embryo, that puts the embryo at harm. So unless that were changed by an act of Congress, biomedical scientists can’t ask questions about the early embryo that has relevance for infertility or birth defects. And so we as a society, at least as the Congress has decided, don’t go there. I hope it changes. I think we are remaining ignorant about some very fundamental questions. Our rate of success with infertility treatment is very, very low. The understanding of the basic biology of birth defects is still very poor, and we can’t study that unless we have the full strength and resources of the federal government, so I hope it does change one day, but I think it’s going to require an evolution of attitudes. You can’t even use the embryos that are created by IVF that are going to be discarded as medical waste. You can’t study those embryos using federal dollars. Only if you make the stem cell lines extracted from the embryos using private dollars can you then transfer them into federally funded research.
The Obama decision is not a complete liberalization of stem cell research policy. It simply expands the access to the more than 1,000 new stem cell lines. So it’s valuable, but it still leaves us with one hand tied behind our back in asking many questions about early human development.
The arguments will be made that now that we have IPS cells and we have adult stem cells, we no longer need embryonic stem cells. Scientists who study these cells don’t agree. There are many questions that remain unanswered about the behavior of IPS cells. Will they be the same as embryonic stem cells? Will they behave in a safe and productive matter? We know that already that adult stem cells don’t give us the same versitility as embryonic or IPS. So I would say, as a scientist and as a physician, it’s far too early to be closing any doors of opportunity. If we want to understand disease, if we want to push the frontiers of medical knowledge, we need all the tools available to us.