In This Episode << SLIDE LEFT TO SEE ADDITIONAL SEGMENTS
Church Health Center
BOB ABERNETHY: Our cover story today is about hope and healing in Memphis, Tennessee, where people of faith are taking on a major national health-care problem. According to the most recent figures from the Census Bureau, 44 million Americans do not have health insurance. Everyone agrees solving that problem will take more than church volunteers, but take a look at what a devout doctor and Memphis’s Church Health Center are doing.
Memphis is famous for music–and poverty. It’s one of the poorest big cities in the country, and that’s why Scott Morris moved to Memphis to live.
Dr. SCOTT MORRIS (Church Health Center): God’s called us all to do our piece in this, and we all have to do our own little small piece, and it’ll work just fine.
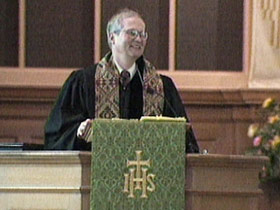
ABERNETHY: Morris’s part-time job is being associate pastor of St. John’s United Methodist Church.
Dr. MORRIS: What does it take to be a disciple of Jesus?
ABERNETHY: Morris’s full-time job is being a medical doctor, the founder and director of Memphis’s successful and revolutionary Church Health Center.
Dr. MORRIS: The mission of the Church Health Center is to reclaim the church’s biblical and historical commitment to care for the poor who are sick.
ABERNETHY: Specifically the working poor, people who earn enough so they do not qualify for Medicaid, but can’t afford private health insurance.

Ms. SHIRLEY SWIFT (Patient): You know, if you don’t have someplace like this, what are you going to do?
Dr. MORRIS: You might cough for six weeks.
ABERNETHY: Morris started the Church Health Center in 1987 by himself with church and foundation backing and 12 patients.
Dr. MORRIS: Let me just listen to your breathing.
ABERNETHY: He persuaded 150 congregations — Protestant, Catholic, and Jewish — to help. He mobilized the medical and philanthropic communities. And today, the Church Health Center has 30,000 patient visits a year, and the price is right.

RECEPTIONIST: And then your charge for today is $10.
ABERNETHY: Except for the homeless, every patient pays a little. The rest of the budget, more than $4 million a year, comes from churches, synagogues, foundations, and the majority from private donors. Morris takes no money from the government.
Dr. MORRIS: It’s not about having the government say, “You have to do what you’re supposed to do.” It is about the people of faith rising up and doing what we are called to do, and that is care for the body and the spirit.
ABERNETHY: The Church Health Center has a small paid staff. All the rest of the work is done by volunteers. They sort pills and keep records. Pharmaceutical companies donate medicine, and hospitals give lab work and take patients. Doctors and nurses in private practice work night shifts after their own workdays are over. But Morris wants no volunteer burnout, so he asks doctors to volunteer only once every three months. The generosity of the volunteers and donors has been essential.

Dr. JAMES BAILEY (Volunteer): I think, very honestly, that it has a little bit to do with the Bible Belt. There’s been a very strong, multidenominational support of this project because people are trying — not always doing a very good job, but they’re trying to practice what they preach.
ABERNETHY: One of Morris’s inventions is an insurance plan so restaurants and other small businesses could get coverage for their lowest-paid workers. Cost: $35 a month, all or most of it usually paid by the employer, and the insured see doctors in their own offices, just like anyone else.
Dr. CHRISTINE MROZ (Breast Cancer Specialist): You look pretty good for having all that surgery just recently.

I don’t even know which ones are Church Health Center and which ones are insurance. I try not to see that, and most of the time, that’s not on the chart.
ABERNETHY: However much the center does provide, there are certain services patients cannot get, for instance, prenatal or maternity care, which is available to the poor elsewhere, and there is no reproductive care. All the practitioners at the Church Health Center say they’ve learned that poverty itself causes sickness of body and soul.
Dr. MORRIS: Poverty drives people to lose hope and to lose a sense of who they are.
Dr. MARY NELL FORD (Church Health Center): I would say 80-90 percent of what we see could be prevented or ameliorated by lifestyle changes. Most of our patients are overweight, hypertensive, diabetic women, and they face horrible health problems because of that.
ABERNETHY: Dr. Morris says half of all the people who come to any primary care doctor have no medical problem.

Dr. MORRIS: Well, it’s not broken, is it?
They come because their life is falling apart, and I can’t fix that with a 15-minute office visit. And I can’t tell you how many people I’ve seen over the years who came saying, “My back hurts,” and in reality, their heart hurts. They have a broken heart.
ABERNETHY: Church Health Center pastoral counselors try to get at underlying psychological and spiritual problems. For this patient, these are family issues now. For many others, they are long-buried victimization.
Reverend KIMBERLEY CAMPBELL (Pastoral Counselor): More than half of the women that I see, maybe as much as 70 percent of the women that I see, have in their histories incest, experience of child sexual abuse, and a lot of what physicians see in their offices are results of the stress of carrying these secrets and this shame. It’s making them sick.

ABERNETHY: Their experience of treating the poor has turned Morris and his colleagues into crusaders for two fundamental changes: new lifestyles for the poor and a new emphasis on prevention in medicine.
Dr. MORRIS: Wouldn’t it be better if we had a health-care system where the doctor’s role was to, in effect, be a Maytag repairman, to try to keep you healthy rather than wait till your body is broken?
ABERNETHY: So Morris turned a former car dealership into the Hope and Healing Center. Donors gave $7 million for the renovation, creating what looks like a spectacular health club. But its director does not like that term.
Ms. LISA VASSER (Director, Hope and Healing Center): It’s not a health club at all. It is a sanctuary for health. We’re not a fitness center, not a wellness center. It’s a place where people can come and literally take care of their spirit or at least think about taking care of their spirit as well as their body.

ABERNETHY: Anyone can join and get a prescription for health, to lose weight and change diet. There are cooking classes with low-fat recipes, mashed potatoes this day made with nonfat dry milk.
Rev. CAMPBELL: Allow yourself to feel the peace of God.
ABERNETHY: There’s also a chapel and a chaplain and regular services of guided meditation.
Rev. CAMPBELL: … living in this present moment.
ABERNETHY: The question, of course, is: If the Church Health Center works so well here in Memphis, could it be duplicated in every other major city? And if so, how far would that go toward meeting the health-care needs of all the country’s working poor?
In Washington, Surgeon General David Satcher praises the Memphis approach, but says the needs are greater than volunteers alone can meet.
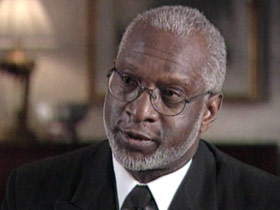
Dr. DAVID SATCHER (United States Surgeon General): I think those kinds of volunteer community programs are great, but I don’t think they’re an answer to the problem. We need to balance health promotion, disease prevention, early detection, and universal access to health care in this country, and it takes public-private partnerships.
ABERNETHY: Morris agrees his center is not the whole answer. For all it’s doing, it’s reaching only about a quarter of Memphis’s uninsured poor. But that’s 30,000 people who were not reached before, and Morris does think his work can be a model.
Dr. MORRIS: Every little piece of what we do, we think, can be reproduced. You don’t need Scott Morris, who’s a physician and a pastor, to do this. What you do need is one person who lives and breathes the idea, who has the commitment and the passion to make it happen.
ABERNETHY: And, day by day, an attitude of mutual respect.
Dr. FORD: I talk to the patient; the patient talks to me; we listen to each other. And that’s the way it should be in every patient-physician relationship.

Ms. MARGARET WARREN (Patient): They don’t know what race or color is. They don’t know anything what age or beauty or ugly is. They just know human beings and a patient that needs them. And that’s why I love coming here.
ABERNETHY: Meanwhile, Church Health Center doctors say their patients have had a profound effect on them.
Dr. FORD: Virtually all of our patients, if anything, teach me about what faith really means. What my patients have been through in terms of loss of children, loss of spouses, personal health problems, health problems in family members, and to come through it with a greater faith and a greater love of God.
Dr. MORRIS: That’s really the power of my experience with patients is that I learn about my own faith from being with people like that. They show me, they teach me, and I would never give that up. Nobody needs to call me for another job. This is what I’m going to do. I’m going to do this until I draw my last breath.
Okay. Well, we’re going to work really hard, and I think with Hope and Healing we can really get things on track.







